by Ulrik Larsen
Glucagon is traditionally seen as a pancreas-specific hormone, but evidence suggests an extra-pancreatic source that responds abnormally to oral glucose in diabetic patients. This study investigates whether the intestine could be responsible for this unexpected glucagon secretion.
To model the glucagon response in pancreatectomized patients, the researchers used a mouse model of subtotal pancreatectomy (Px) to further explore this phenomenon in vivo. Px mice rapidly developed hyperglycemia, ketonemia, and a paradoxical increase in glucagon secretion in response to oral glucose. Histology showed fibrosis and no α-cell regeneration in the remaining pancreas, and isolated islets failed to secrete glucagon, suggesting another tissue as the source.
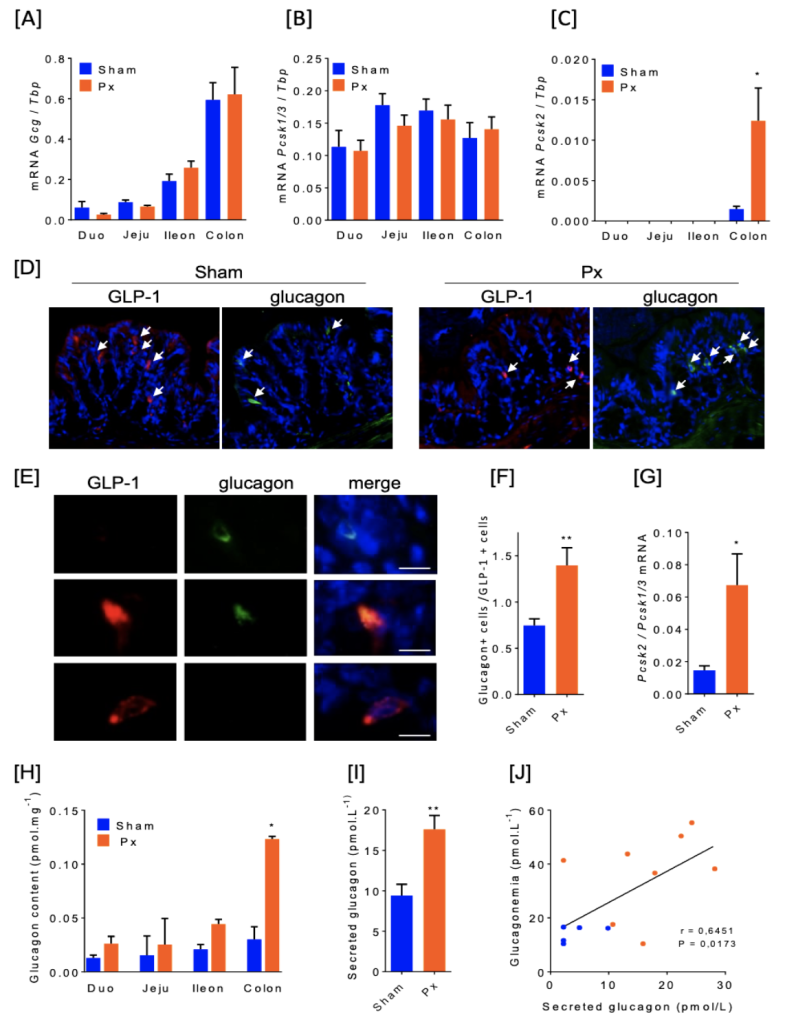
Focusing on the gut, the researchers found that while proglucagon (Gcg) expression was highest in the colon under normal conditions, pancreatectomy significantly increased colonic expression of PCSK2, the enzyme required for processing proglucagon into glucagon. Furthermore, glucagon content in the colon increased fourfold in Px mice compared to controls, and an ex vivo secretion assay revealed that the colon actively released glucagon. The degree of colonic glucagon secretion correlated with elevated glucagon levels in vivo, supporting the idea that the intestine can serve as a stress-mediated glucagon source after pancreatic resection. These findings challenge the traditional view of glucagon as a purely pancreatic hormone, highlighting the need to explore the molecular mechanisms behind the colonic shift in glucagon production and its potential role in dysregulated glucagon secretion in diabetes.
One important consideration for this proposed mechanism is whether this adaptation is a short-term or long-term response, and whether it is primarily an inflammatory reaction rather than a glycemic-driven adaptation. The study was conducted within two weeks of surgery, leaving open the question of whether PCSK2 expression and glucagon secretion would persist over time or revert to GLP-1 production. Additionally, while the researchers used specific primers for glucagon detection, further validation with another highly specific techniques to use targeted mass spectrometry would help confirm whether the detected glucagon is truly identical to pancreatic glucagon or if other proglucagon-derived peptides contribute to the observed effects.
Figure:
Adaptation of the gut after subtotal pancreatectomy results in an increased glucagon production and secretion by the colon
Continue your reading here:
Jarry, A.-C., Le Beyec, J., Bado, A., Gautier, J.-F., Riveline, J.-P., Blondeau, B., Guillemain, G., & Le Gall, M. (2024). The colon is an extra-pancreatic source of glucagon: Demonstration in a mouse model of pancreatectomy. bioRxiv. https://doi.org/10.1101/2024.12.23.630024